A nationwide physical therapy business is renowned for eliminating chronic pain. One unique aspect of this business is that it eliminates pain not by manipulation but by providing clients with expertly selected sequences of exercises that address problems in their functional anatomy. In effect, the business helps people fix themselves and teaches them to maintain their musculoskeletal function for pain-free life.
The business has dozens of clinics with many more therapists. Its expertise comes primarily from its founder and a number of long-time employees who have learned through experience. We have been engaged to assist with several challenges on several occasions.
One of those challenges was helping to extract the expertise of the founder. Actually, the challenge of extracting the expertise of the founder was second-order. The first-order challenge was to make the business scalable beyond the constraints of the founder’s physical availability. Trained physical therapists found it difficult to comprehend the founder’s technique. And those that grasped it to varying degrees applied it inconsistently, requiring continuing supervision by the founder.
We were successful in doing this using traditional techniques, such as protocol analysis (or perhaps, more precisely, what Newell and Simon called “information processing psychology”).
The founder had identified a number of key patterns based on functional anatomy that tended to lead to certain kinds of compensation and pain. For example, if one hip is tilted more than another, there is a torsion on the lower spine. If the hips are tilted forward, there is an increase in lumbar curvature. If there is rotation of the upper leg, there is increased stress on the knee when walking. Any of these things will lead to further compensation and, eventually, pain and, perhaps, injury.
- To put it simply, the cure is to reverse the process and restore proper muscular function and proper posture.
The business used the resulting system[1] to expand nationwide and internationally over the last two decades. But the founder continued to learn while the system did not. And the effectiveness of what emerged as “the method” remained anecdotal.
Twenty-five years ago, we simply figured out what the founder perceived and how he thought about it to choose exercises. In the decades since, the company has tried to simplify that knowledge into a small number of patterns they call “conditions”.
The advantage of having conditions is that it is easier to teach a therapist to recognized them. The disadvantage is that it reduces personalized exercise sequencing to selection among a small number of preordained “menus” of exercises. In practice, this results in longer, perhaps less-effective, exercise sequences than those of an expert who can see the effect of each exercise and “prescribe” a sequence that is most efficaciously focused on any specific client.
Optimizing the efficacy of physical therapy
As described previously here, the data captured by the initial system (which was deployed prior to widespread availability of digital cameras and the Internet) was subjectively interpreted by therapists. Replacing Polaroids with digital pictures improved the workflow but not the objectivity of posture data. More recently, vision and balance sensors provide objective data from digital images and color/depth cameras, as well as objective data on left/right and front/back weight bearing per foot.
With our current capabilities, a self-learning exercise recommendation system and clinical management system is ready to optimize the efficacy of physical therapy.
This post discusses factors that we have incorporated into a model of exercise selection based on objective longitudinal data. The recommendations were initially seeded using expert knowledge to formulate structured equation models that we adapt using statistical techniques, including Bayesian data analysis, and some neural techniques, which we can only touch on here due to the length of the introductory discussion.
For various reasons, including some that follow, we do have not pursued automated exercise prescription. Our objective is expert recommendation of exercises by a continuously improving physical therapy (PT) system based on clinical evidence. Given a few highly ranked recommendations, therapists or clients themselves can select an exercise (or veto a recommendation, as discussed below).
These recommendations have been used successfully in many thousands of physical therapy sessions.
And our client can demonstrate, objectively and quantitatively their efficacy.
Expert physical therapy
An expert therapist selects the most appropriate exercise at a point in time. This is not a direct mapping from posture to exercise selection. An expert therapist also considers any symptoms (e.g., pain) and the client’s function (e.g., how strong or flexible they are).
Physical conditions and fitness
For example, someone who just had their knee replaced or who has severely arthritic wrists would not want to do cats & dogs, even if it would be otherwise indicated by scoliosis or having just finished a seated spinal twist (to minimize the risk of back spasms in someone with complex or excess spinal curvature). As another example, someone who has ankle or wrist joint symptoms would not be a good candidate for the downward dog, nor would be someone not strong enough to hold half their weight on their hands.
Symptoms
In my experience, most therapists are extraordinarily compassionate. If a client is hurting, there is a tendency to treat the symptom rather than to more directly attack the cause. This brings relief but risks dissatisfaction when the pain returns shortly thereafter. Attacking the cause seems less compassionate in the short-term but can be more compassionate in the days following a visit to a clinic. Moreover, alleviating symptoms frequently takes more time than reducing causes.
Treatment
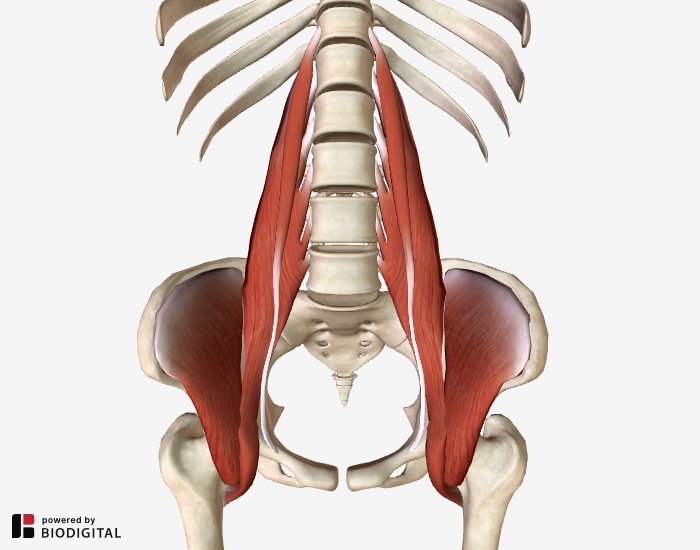
One technique for reducing several types of pain (especially lower back, hip, and some knee pain) is to perform a passive stretch of muscles in the lower back, hips, and upper legs. For example, the supine groin stretch relaxes the iliopsoas (aka hip flexors). But the supine groin puts just enough stress on the psoas that it can trigger pain or back spasms in people with symptoms or significant dysfunction. In those cases, the static back may be effective, but it can take a while and, like all passive stretches, not take enduring effect.[2]
Helping with therapy vs. automating therapists
As we mentioned above, our objective is an expert PT system that recommends exercises. We leave it to therapists or clients to decide which exercise is right for them. As they indicate conditions or symptoms that contradict recommendations, future recommendations should consider that feedback and how it may change over time (i.e., an artificial knee permanent precludes some exercises, shoulder dislocation risks may improve over time, and pain can be quite transient). Therapist can also indicate how difficult and/or effective exercises (as can clients from their laptops or mobile devices when they perform exercises at home).
Prerequisites to self-learning decision support for PT
An expert PT system requires a variety of knowledge in order to recommend and learn:
- how muscles are attached to bones
- how muscles and bones are involved in articulations of joints
- how muscles are typically engaged in and affected by exercises
- how joints are positioned and/or articulated in exercises
- how weight is borne in exercises and positions
- how conditions or symptoms pertain to muscles, bones, and joints
Such knowledge is readily available and well-known by skilled physical therapists.
For example, the iliopsoas attaches to the lumbar spine, ilium, and the femur. It attaches medially on the femur such that when engaged it tends to rotate the femur externally while lifting the femur to the anterior (i.e., flexion of the hip). The static back shortens the iliopsoas (through passive flexion of the hip) thereby relieving tension on the pelvis and lumbar spine. The supine groin passively stretches the iliopsoas. Weight is distributed along the back in each case. As another example, the downward dog demands dorsiflexion (an ankles and hands), knee extension, hip flexion, thoracic extension, shoulder flexion, and elbow extension with 25% of body weight borne per hand, wrist, elbow, shoulder, knee, ankle, and foot. The muscles involved in the elbow, shoulder, and knee articulations are isometrically engaged and those involved in dorsiflexion at the ankle (in particular) are aggressively stretched.
Given that knowledge, there are some core aspects of physical therapy that a system should understand before it may be considered expert, such as:
- different types of muscular dysfunction (including imbalances)
- how muscular function or dysfunction relates to posture and balance
- how deviations from ideal posture and balance manifest pain
- how stretching and/or strengthening muscles affects posture and balance
- how similar exercises performed in different positions may vary in effect
- when passive stretching may be preferable to active stretching
- how to optimize the effect of therapy given limited time
- how to optimize therapy before or after certain types of physical activity
- certain conditions counter-indicate certain articulations and/or weight bearing
There is too much practical knowledge about PT to contemplate here, though. Here we want to address how this initial knowledge is used and how it facilities self-learning and evidence-based physical therapy.
Physical therapy modelling basics
Here is an abstract model of exercise recommendation:
- Observe posture (i.e., obtain the angles of articulation of all joints[3]) and balance (i.e., obtain left/right and front/back weight distribution per foot).
- vision is important here in that it eliminates judgements that vary across therapists[4]
- Compute longitudinal data from observations along with information about exercises performed (especially sequentially with observations before and after each exercise and/or with feedback per exercise).
- without vision obtaining objective data before and after each exercise is impractical
- Treat the observations and longitudinal data as inputs in a model of functional anatomy comprised of (derived and/or latent) variables of anatomical function (or, equivalently, dysfunction).
- important since, commonly, multiple muscles are involved in articulation or muscles are involved in multiple articulations (including isometrically holding a joint steady against some force)
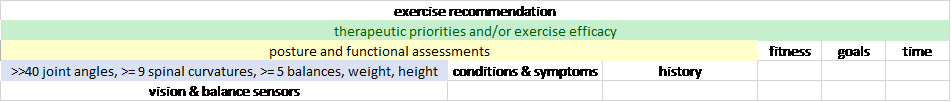
- Treat conditions or symptoms, fitness, goals (e.g., goals, such as an upcoming activity) and psychological factors (e.g., motivation, pain tolerance) along with the foregoing as inputs in a therapy model (e.g., prioritized treatment objectives).
- Treat the longitudinal data and the model of anatomical function, along with conditions or symptoms, and fitness as inputs into a model of exercise efficacy per exercise.
- Treat the foregoing (i.e., longitudinal observations and variables of anatomical function, exercise efficacy, and treatment objectives) as inputs to exercise recommendation.
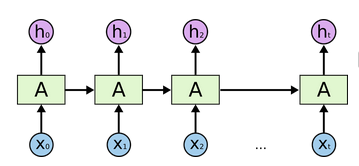
It may be helpful to consider the foregoing as defining a structural equation model or a deep learning architecture with the following levels or layers (roughly speaking):
On the left, the raw data is transformed into anatomical data. The raw data is preserved for future analysis, such as using improved vision but is not used directly at higher levels.
Posture and functional assessments are based on that anatomical data (including its longitudinal history[5]) and, to varying degrees, on a client’s persistent conditions or symptomatic severity.
Therapeutic priorities and exercise efficacy can be viewed as two distinct models which share as inputs the posture and functional assessments, conditions & symptoms, longitudinal history, and the client’s fitness.
Unlike therapeutic priorities, exercise efficacy is less directly dependent on client goals and time available for therapy. Exercise recommendation, on the other hand, is dependent on everything involved in the therapeutic priorities.
As this post is running long, we’ll stop here for now, after just this brief word about selecting sequences of exercises…
It turns out that one exercise can be much more effective if performed after other exercises. For example, depending on a person’s anatomical function, a crossover stretch can make a runner’s stretch (or scissors hamstring stretch) much more comfortable and effective. As another example, a quad stretch can help before a downward dog. These examples show how tight but ancillary muscles can interfere with exercises. They show that many factors affect expert exercise selection and sequencing. Although not the only approach to learning when exercises are efficacious, to those who are inclined towards neural networks or deep learning, they may suggest a recurrent neural network (RNN) approach for some of the layers above.
[1] Also see https://ctpainfree.com/pain-free-in-5-easy-steps/
[2] For example, this page discusses what to do when the static back is not doing the trick. Ceteris paribus, active exercises are more productive than passive ones.
[3] perhaps treating the spine as several segments or characterizing lumbar/thoracic/cervical curvature by a degree or excessive curvature or straightness in the anterior/posterior and lateral planes
[4] including exaggerations which are common when communicating assessments to clients
[5] note that longitudinal history (which is redundant for clarity) may be global or per patient (or per cluster of similar circumstances, such as in the “conditions” discussed above)